The NHS: a love-hate relationship
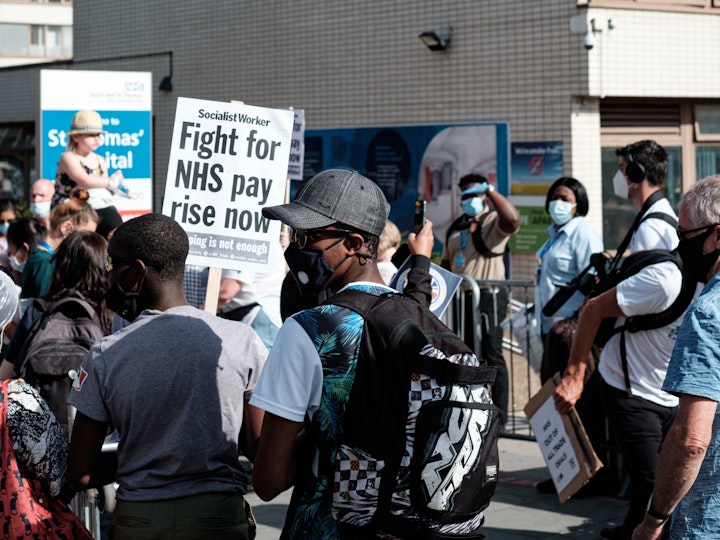
With the junior doctors’ strikes still making headlines across the country Professor David Pendleton, Professor of Leadership, says now is the time for radical ideas and courageous leadership.
Walking on a beach in Australia I passed a restaurant displaying a sign which read ‘we serve good food, fast food and cheap food – which two would you like?’ This impossible triplet is not alone.
In fact, there is an impossible triplet at the heart of the NHS which may even have caused our current ‘love-hate’ relationship. The triplet is: quality, access and affordability. We want high quality care consistent with the highest professional standards and the equal of our international peers. We have charged the Care Quality Commission with monitoring this. We want minimal waiting times (access) and are horrified that there are now over 7 million people waiting for treatment. We also fear our healthcare is unaffordable. When the NHS was created it consumed around 4% of GDP. It is now up to 10% and rising.
Before the imposition of standards for waiting times, quality and affordability were balanced by allowing waiting times to increase. But waiting was deemed increasingly unacceptable and standards were created to monitor and target the NHS’s access to care, so introducing the impossible third element of the triplet. We now face an NHS that is on its knees.
How does the UK compare?
The UK spends roughly £168bn on health and social care which some estimate to be 18% less per capita compared with the other prosperous European economies. We certainly have fewer hospital beds than almost any other rich country. Instead, the government has turned muddling-through into a continual round of kicking the can down the road with short-term injections of cash which can never do more than relieve pressure temporarily.
The government looks at the cost-of-living crisis and recoils at the level of tax increases that would be needed to match the levels of healthcare spending of our European peers. The Conservatives are held back by their right wing which want to see taxes come down rather than increase. They want to be the party of low taxes. Labour are nervous about turning their poll lead into votes at the next general election and fear their former reputation as a tax and spend party, running up national debt.
Who is paying the price now?
First, there are the seven million people paying by waiting for treatment. Second, the staff in the NHS are paying through low wages and stress. My daughter Katie, a GP, put it brilliantly. She asked ‘the system is broken so why are we breaking ourselves trying to fix it?’ As a former Trustee of the Royal College of General Practitioners, I know she was speaking for most of her colleagues and that is why so many young GPs are leaving the profession.
This level of frustration is felt by patients, clinicians and managers alike. The clinicians point out that the nation applauded them on Thursday evenings in the pandemic but its government is reluctant to uplift their pay even by the level of inflation. Patients are angry that they cannot get through to their GP practices on the phone and then, if they can book an appointment, must wait weeks for it.
On arrival at the surgery, they find an empty waiting room and therefore assume that demand is low and the doctors are not working very hard. The reality is that, on the contrary, GPs are typically working 12-hour days and treating more patients with fewer doctors than ever before.
Fixing the NHS will require radical and innovative thinking
The situation is perilous for all concerned and anxiety about the imminent collapse of the service is sounding less like crying wolf and more like a statement of the blindingly obvious. It cannot continue but fixing it will require radical possibilities to be considered. An entire herd of sacred cows may need to be euthanised. We can treat everyone but maybe not for everything, so what do we not cover? Or maybe we can treat everything but not for everyone, so who do we exclude? Or maybe charges need to be considered seriously rather than dismissed out of hand. Possibly funding through taxation needs to be twinned with funding through insurance. Maybe charges for each consultation could be introduced, or charges for missed appointments. Or maybe care is free for those who cannot afford to pay but paid for by those who can.
There are offered wide-ranging reasons for the NHS’s unsustainability. The causes are many and varied. They include the demographics of our aging population, the soaring cost of treatments, the relentless rise in expectations of cures for all ills and the like. On the upside, there is the possible positive contributions from advances in technology and breakthrough innovations such as virtual wards but the overwhelming pressures on the service call for new thinking and new leadership.
Clearly this is a matter for all of us. It cannot be left to the leadership of politicians alone since their horizons are seldom longer than a few years and the extent of the changes required to make a significant difference in the fields of health and social care will take longer than that. There are several initiatives that are currently under way to help address these matters. The Times Health Commission is meeting during 2023 and will report in 2024. It is looking at health and social care as an integrated system. The Institute for Public Policy Research has launched an initiative to consider the relationship between a fairer society, a healthier society and a more prosperous society. Theirs is an initiative backed by contemporaneous research including the investigation into the wishes of the people of our country: bottom-up policy making.
At Henley Business School, we are planning to contribute to the discussion of the purpose of the NHS. We will ask what the health service is for, what we want it to do for us and what might need to change to bring this about. We will meet in June and offer some insights for debate.
Leadership starts with setting strategic direction. Its first contribution is the identification of a clear purpose to meet a carefully understood need. In the case of health and social care this involves consideration of the kind of society we want to create in our country and the implications for how we fund and provide the care we all need at some stage in our lives.
As a nation, we all have to get our thinking caps on to break out of the impossible triplet of access, quality and affordability. To rekindle our love affair with the NHS, we need radical, imaginative thinking based on a thorough understanding of the needs and wishes of our people.

